Post-meal blood sugar spikes increase health risks
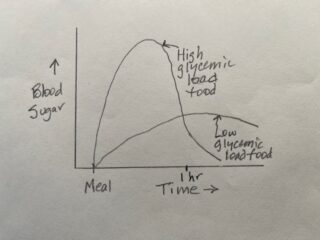
Reducing excess blood sugar (hyperglycemia), especially after meals, reduces the risk of cardiovascular disease. A review linked hyperglycemia to increased risk of complications of type 2 diabetes. Physicians use glycated hemoglobin (HbA1c) to measure blood sugar over the previous 2-3 months. The American Diabetes Association recommends that persons with type 2 diabetes keep their HbA1c at or below 7.0 percent, while the American Association of Clinical Endocrinologists recommends 6.5 percent. While most physicians focus their attention on fasting blood sugar concentration, post-meal blood sugar concentration may be a better measure. While medications can help reduce blood sugar to safe levels, altering diet that emphasizes low-glycemic load carbohydrates can greatly reduce post-meal blood sugar spikes.
Physicians with the San Luigi Gonzaga Diabetes Study reported in 2010 that higher levels of post-meal blood glucose predicted greater risk of heart attack after five years of follow-up. The physicians confirmed and expanded their results after 14 years of follow-up. Higher levels of post-meal blood glucose (2 hours after lunch) and HbA1c analyzed together predicted significantly increased risks of cardiovascular events (45 percent for post-meal blood glucose and 72 percent for HbA1c) and mortality (85 percent for post-meal blood glucose and 90 percent for HbA1c). Reducing HbA1c levels with better diet and/or medication to lower daily blood glucose and reducing post-meal blood glucose levels to avoid sharp blood sugar spikes (with better diet and exercise) appear to greatly reduce subsequent risk of cardiovascular events and premature death. Interestingly, fasting blood glucose levels (the blood sugar test that doctors typically recommend) did not predict risk of cardiovascular event or mortality.
Glycemic load, exercise, and monitoring program
Medications and lifestyle changes comprise the therapies for type 2 diabetes. The American Diabetes Association typically recommends weight loss abetted by lower intake of high-calorie foods and increased physical activity as the lifestyle changes. Alas, only a modest fraction of people are able to lose weight permanently. Recent research suggests that improving diet through reducing intake of high-glycemic load carbs can help people with type 2 diabetes manage their blood sugar levels.
Researchers at the University of Virginia developed the Glycemic load, Exercise, and Monitoring (GEM) program as an alternative approach to managing type 2 diabetes. The monitoring portion of the program sought to educate participants about how foods affect blood glucose levels, motivate participants to learn which food choices raise or lower blood sugar, and motivate participants to eat better and engage in more physical activity. A preliminary randomized, controlled trial included 55 people with an average of 55 years of age with type 2 diabetes diagnosed within the previous 5 years. Participants were randomized to routine care or to the GEM program, which provided five classes to orient participants to the program with a manual and by learning to use a provided blood glucose monitoring unit.
At 6 months from baseline, participants in the GEM program had significantly lower HbA1c (1.0 percentage point) than participants in routine care (0.1 percentage point). GEM outperformed routine care on a number of other measures: better knowledge of type 2 diabetes, lower intake of high-glycemic foods, fewer total carbs, fewer calories, lower body weight, greater HDL cholesterol, higher perceived quality of life, fewer common concerns about diabetes, and greater diabetes empowerment. All this without increasing diabetes medications. Overall, the GEM program yielded better results medically and psychologically than routine care.
Researchers at the University of Virginia developed the GEM program that minimizes blood sugar spikes of persons with type 2 diabetes with follow-up to 3 months. The results from another 10 months of follow-up confirm earlier results. From baseline to 13 months, three slightly different GEM groups (combined for analysis) showed a significant decline in HbA1c (-0.5 percentage point), while the weight loss group showed a non-significant -0.2 percentage point decline. Compared to the weight loss group, the GEM groups showed greater sustained diabetes empowerment, diabetes knowledge, and reduced carbohydrate intake. The overall message: GEM was either better than or equivalent to weight loss in managing type 2 diabetes. The positive effects of GEM may have arisen from empowering participants to monitor their blood sugar, increasing their knowledge of type 2 diabetes, shifting their diet toward low-glycemic load carbs, and increasing physical activity.
What to do
If you have been diagnosed with pre-diabetes or type 2 diabetes, it’s in your best long-term self-interest to learn how to manage your blood sugar. Keeping your blood sugar in a healthy range largely arises from eating healthier (especially low-glycemic load) foods, increasing your level of physical activity, and monitoring your glucose. You may be able to enroll in a diabetes management program that suits you through your primary medical provider. You insurance my cover the cost of the program.